Am I seeing a physician associate or a doctor?

In recent years, the NHS has expanded the use of 'medical associate' roles to help tackle staff shortages and improve access to care. One of these roles is the Physician Associate (PA).
With plans to employ 10,000 physician associates by 2037, we look at how aware patients are of PAs and how NHS staff and medical regulators can improve their understanding and experience.
What is a physician associate?
Physician associates are healthcare professionals who work under the supervision of a senior doctor and can assess, diagnose, and treat patients within certain limits.
They don’t prescribe medication or request X-rays, and they are supposed to supplement - and not substitute – fully qualified doctors.
PAs are not a new role.
Physician Associates have worked in England since the early 2000s, but the number employed in the NHS has grown significantly in recent years.
The Faculty of Physician Associates found that 2,833 PAs were working in England in October 2022, more than double the number recorded three years earlier.
The previous Government asked the General Medical Council to take on formal regulation of PAs alongside its main role of regulating doctors. This move aimed at assuring patients, clinicians, and employers that PAs have the knowledge and skills to work safely and that they can be held to account if serious concerns are raised.
With the regulation of PAs due to start at the end of 2024, we have looked at what patients have told us about PAs and the lessons the NHS and the GMC can learn from our evidence.
What patients and the public think
It is challenging to accurately gauge people’s experience and understanding of physician associates. There are still not many PAs practising in the NHS, and there is little national data about which services employ them and in what capacity.
To establish the first national picture of the patient experience of this new role, we commissioned a poll of 1,914 adults living in England*. We also spoke with local Healthwatch services about the stories people had shared with them.
Key themes
General awareness is mixed
In our polling, we found a mixed picture on awareness of physician associates.
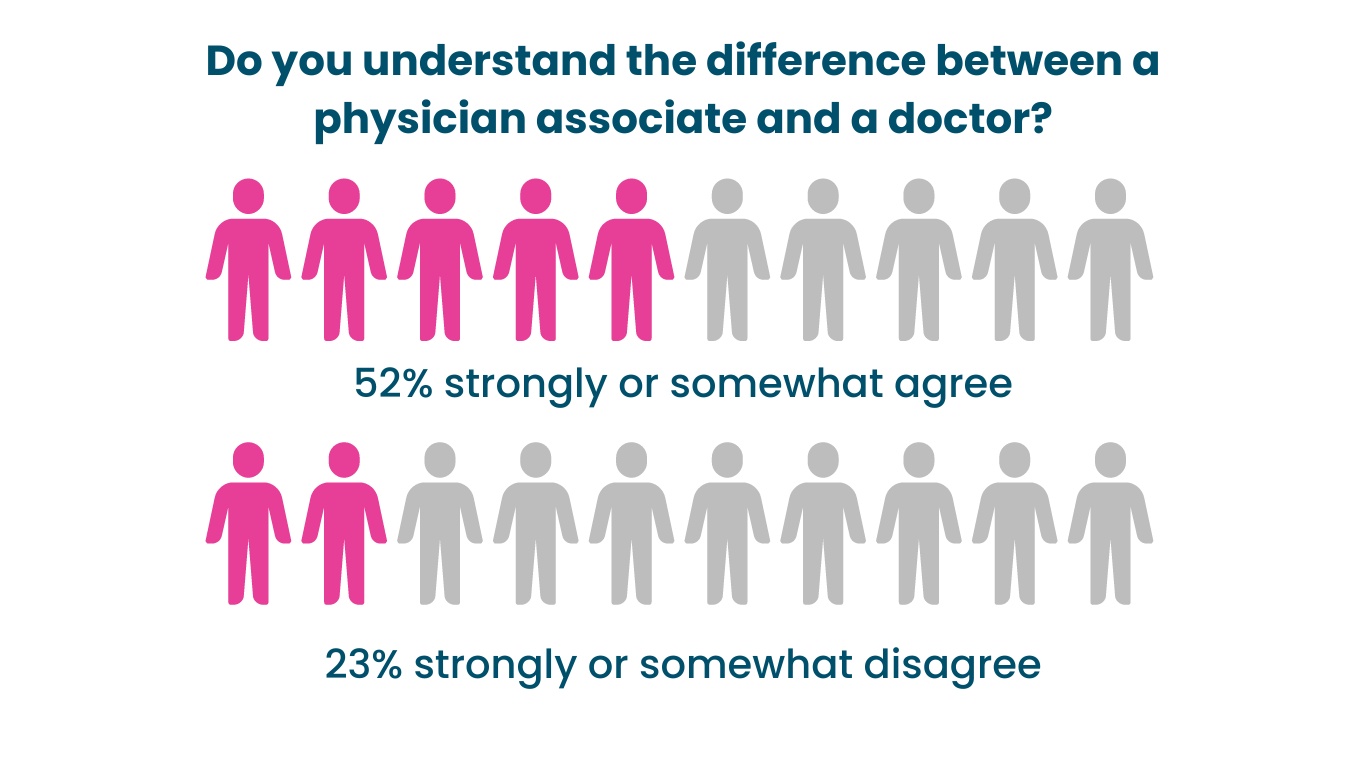
In our polling, we found a mixed picture on awareness of physician associates. Over half of those surveyed (52%) agreed or strongly agreed that they “understood the difference between a physician associate and a doctor”.
However, there were differences when it came to age.
Respondents aged between 18-34 were more likely to agree with the statement (58%) than those in older age groups (47% of 34–54-year-olds, and 49% of those aged 55+ agreed).
Some local Healthwatch explained that while patients might have heard of PAs and understood that they were not doctors, understanding what they can and can’t do is more limited.
In many cases, patients were not aware of the local presence of PAs and often only found out about the role when given an appointment with a PA.
Knowing who you are seeing is key
Where people knew they had received care from a physician associate, their experiences tended to be positive. People particularly valued that they could have their needs addressed quickly when they saw a PA.
However, we heard about several cases where patients were not made aware of who they were seeing before or during their appointment. In some instances, patients had specially asked to see a doctor but were instead assigned to see a PA.
However, we heard about several cases where patients were not made aware of who they were seeing before or during their appointment. In some instances, patients had specially asked to see a doctor but were instead assigned to see a PA.
Five steps to improve clarity.
In partnership with the Patients Association and National Voices, we’ve made five recommendations to policymakers and regulators about how they can better support the roll out of PAs. A commitment to clarity about the PA role underpins these recommendations.
1. Clarity in direct patient care
Practising physician associates and those in training must explain their role to all patients they see. Providers of education and training, including medical royal colleges, should make clear that informing patients about roles and responsibilities is core to providing high-quality care.
2. Clarity on choice
While PAs can provide high-quality care and improve patient access for more straightforward health problems, national and local NHS organisations must make clear that patients have a choice e to request an appointment with a fully qualified doctor if they prefer.
So people can make an informed choice, services should tell patients before an appointment:
- The types of clinicians available to see them
- The lengths of time they may have to wait to see different professionals, and
- If they see a physician associate, the PA may have to refer the patient to a GP or other senior doctor if the patient’s problem falls outside their scope of practice.
3. Clarity on training and regulation
In our polling, we found that the factor which made the public most confident in the person providing their care had “their skills and knowledge regularly reassessed”.
National bodies, including the Faculty of Physician Associates and the General Medical Council should be clear about the scope and content of the initial training of PAs and their ongoing assessment and revalidation.
4. Clarity of communication
Given the increasing use of new roles in services, NHS England and other national bodies should adopt a proactive approach to communicating with the public in this area.
Alongside broader awareness campaigns, Integrated Care Boards should set up patient forums to explicitly examine the deployment of new workforce roles. Patients and their representatives must be centrally involved in all future discussions about the use of PAs and other new roles.
5. Clarity on effectiveness
NHSE and the GMC should commission a formal evaluation of patient experience of physician associates in GP and hospital settings. This research would help to learn lessons to inform the expansion of this role and provide assurance that PAs are being used appropriately and are not as substitutes for fully qualified doctors.
Want to learn more about physician associates?
Find out what care they can offer you and how their role differs from fully qualified doctors in our advice article.
*Healthwatch England commissioned a representative survey on public attitudes to Physician Associates. The poll ran as part of its weekly Omnibus survey. People responded between 13 and 14 April 2024.


